Hormone Disorders
Hormonal dysfunction is a common cause of infertility.
The most common reproductive disorder in young women is polycystic ovary syndrome (PCOS).
Irregular ovulation can lead to irregular menstrual cycles, disruption of a normal lifestyle, excessive blood loss, anemia, fatigue, precancerous lesions in the uterus and infertility.
Hormones are important for your body and your fertility. They are the body’s neurotransmitters and control a number of biological processes. Further down the line, they also control your reproductive physiology. If you suffer from hormonal disorders, this can reduce your fertility
At Footsteps To Fertility Centre, we focus on the woman’s hormone balance. We analyze your hormones in the laboratory to get a picture of your situation. If you have a hormone disorder, we look at the treatment options that we can offer you.
Menstrual cycles may be irregular in the first few years, but afterwards they should be in a regular monthly pattern. It may be convenient not to have periods, but the consequences can be devastating such as estrogen deficiency, bone loss, infertility, endometriosis and endometrial cancer.
If your menstrual cycles are irregular, you should be evaluated by a reproductive endocrinologist to identify the cause and start treatment as soon as possible.
How do hormone disorders arise?
The body is a complex machine, and so is the hormonal system. Even small changes in the body are enough to affect the hormone balance. An imbalance could arise or be triggered by a pituitary or thyroid gland disorder. It could also be triggered by a disturbance of hormonal neurotransmitters such as Gonadotropin-releasing hormone (GnRH). It is a neurotransmitter that controls the production of sex hormones in the pituitary gland.
There are three reasons why neurotransmitters can indirectly affect a woman’s fertility:
- Egg maturation can be disturbed
- You might not ovulate
- Development of the corpus luteum/production of progesterone might not occur.
- Your BMI can also trigger a hormonal imbalance: This could occur if you are very under-or overweight. If there are big major fluctuations in your weight, or if you are stressed or on medication. In rare cases, it could be triggered by fibroids.

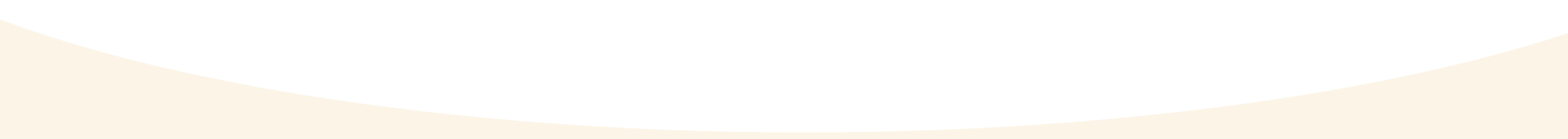
Polycystic Ovarian Syndrome (PCOS)
Global Women Connected. Image source: Female Disorders. Accessed via https://www.globalwomenconnected.com/womens-health/female-disorders/
Polycystic ovary syndrome (PCOS) is the most common reproductive disorder in women of childbearing age.
It is a result of ovarian dysfunction that manifests with irregular periods or no periods (irregular ovulation or no ovulation) and varying degrees of increased androgen effects (i.e. high testosterone or increased hair growth and/or acne) as well as polycystic appearing ovaries (multiple small follicles in the ovaries).
PCOS is a result of ovarian dysfunction that manifests with irregular periods or no periods (irregular ovulation or no ovulation) and varying degrees of increased androgen effects (i.e. high testosterone or increased hair growth and/or acne) as well as polycystic appearing ovaries (multiple small follicles in the ovaries).
At Footsteps To Fertility Centre, we provide support to women diagnosed with PCOS to help them overcome the syndrome and decrease the impact of its associated health problems.
How is PCOS diagnosed?
PCOS is diagnosed by the inclusion of any two of the parameters above, along with the exclusion of other diseases that would present with similar findings.
There is no single test or symptom that would indicate that a person has the disease, but the diagnosis of PCOS is made by a combination of symptoms and blood testing.
It can be associated with other diseases, such as thyroid disease and elevated prolactin hormone levels (the hormone that makes breast milk). Women should be tested for the presence of these disorders if they have PCOS-type symptoms.
Additionally, PCOS patients are at an increased risk for pre-diabetic conditions that can be diagnosed by an elevated insulin level and/or elevated glucose level (glucose intolerance) or even may have diabetes at the time of the diagnosis of this condition.
PCOS Treatment
If the initial workup is diagnostic of PCOS and other diseases are all eliminated by testing, the treatment options are discussed.
Our goal is to provide individualized and effective care, diagnosis and treatment for all women with polycystic ovarian syndrome.
PCOS and Menstruation
Lack of ovulation can lead to an abnormal overgrowth of the uterine lining (endometrial hyperplasia), which increases the risk of uterine cancer.
Menstrual abnormalities can be treated with medications that might include oral contraceptives to regulate the menstrual cycle.
It is therefore very important to screen patients for diabetes at the time of diagnosis of PCOS. Patients who are overweight or obese are at a higher risk for having or developing diabetes in the future.
PCOS and Hormones
The goal of PCOS treatment is to decrease the amount of androgens in the bloodstream, thereby decreasing the clinical effects of androgens on the body such as facial hair growth and acne. The most common treatment is low-dose oral contraceptives. Oral contraceptives decrease androgens in a variety of ways.
For PCOS and facial hair, it is recommended to combine medical treatment with mechanical hair removal methods such as electrolysis, waxing, or laser hair removal.
PCOS and Insulin Resistance
Insulin resistance and hyperinsulinemia (elevated blood insulin levels) are common in women with PCOS.
These metabolic abnormalities can lead to impaired glucose tolerance and Type 2 diabetes mellitus. Some women achieve positive results by going on the type of diet used for diabetes prevention.
Metformin, an insulin-sensitizing medication, is used for the treatment of patients with PCOS. The goals of treatment include improving insulin resistance and lowering insulin levels. An improvement in ovulatory function can also be obtained.
PCOS and Fertility
Women with PCOS are either oligo ovulatory or anovulatory, meaning that they ovulate less often than normal or not at all. If ovulation does not take place, there is no opportunity for egg-sperm interaction and pregnancy to occur. The goal of treatment for infertility in PCOS is to cause ovulation to occur predictably.
Surgical treatment of PCOS
Surgical treatment of PCOS involves the destruction of some of the ovarian tissue (laparoscopic ovarian stromal cauterization) to allow ovulation and regular menstrual cycles.
This type of treatment is no longer preferred because of the high success rate with the medical approach.
In some cases, the surgical approach can be useful, but this type of treatment should be individualized.
Surgical treatment does not improve metabolic parameters (such as elevated insulin or glucose levels) and also does not decrease the risk of diabetes.
If ovulation or pregnancy is not attained with these more conservative treatments, they can be combined with gonadotropin therapy (FSH or human menopausal gonadotropin – HMG – injections. However, gonadotropin therapy may include side effects such as increased multiple pregnancy rates and ovarian hyperstimulation syndrome (OHSS).
Weight loss and exercise should be routinely recommended to patients with PCOS because most patients tend to be overweight or obese.
Weight loss of 10-15% of the body weight is sufficient enough to allow ovulation in most cases.
Additionally, the risk of developing diabetes, high cholesterol and heart disease also significantly decreases with weight loss and establishment of normal weight.
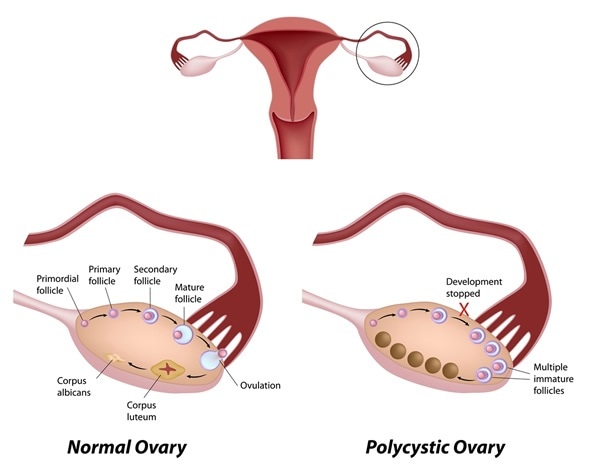
Thyroid Disease
Dr. Richard Payne. Image source: Flickr. Accessed via https://www.flickr.com/photos/182247066@N05/
Thyroid disease is common in reproductive age women and is observed at an incidence of approximately 1%.
Both hyperthyroidism (increased activity) and hypothyroidism (decreased activity) can be associated with reproductive problems.
The most common problem encountered with thyroid disease related to reproduction is dysfunction in ovulation.
Most patients with hypothyroidism will not ovulate and have infertility, but some may ovulate irregularly and conceive spontaneously.
If maternal hypothyroidism is untreated in pregnancy, it may have significant adverse effects on the fetus, such as mental and physical disability.
Hyperthyroidism can also result in ovulatory dysfunction and eventually infertility, with other adverse effects if left untreated.
At Footsteps To Fertility Centre located in Nairobi, Kenya, we are devoted to providing prevention and treatment of Thyroid disease through excellent professional-clinical care and education to patients who have the condition.
Types of Thyroid disease
- Hypothyroidism is defined as high thyroid-stimulating hormone level (TSH) and low thyroid hormones (T3 and/or T4). It can cause ovulation problems, infertility, and is also associated with recurrent pregnancy loss. Hypothyroidism is due to an autoimmune reaction, and when goiter (enlargement of the thyroid gland) is present, it is called Hashimoto’s thyroiditis.
- Hyperthyroidism is defined as a suppressed/low TSH level and elevated thyroid hormones (T3 and/or T4). Two causes of hyperthyroidism are Graves’ disease (toxic diffuse goiter) and Plummer’s disease (toxic nodular goiter). Plummer’s disease is encountered in postmenopausal women who have had a long history of goiter.
Graves’ disease is defined as hyperthyroidism, exophthalmus (protrusion of eyes) and pretibial myxedema (swelling in the legs), and is believed to be caused by autoantibodies.
Symptoms of Hypothyroidism and Hyperthyroidism Disease
Some of the symptoms of hypothyroidism are cold intolerance, constipation, low energy, fatigue, water retention, slow speech, but in some cases patients may be totally asymptomatic.
Subclinical hypothyroidism is defined as an elevated TSH level with normal thyroid hormone concentrations (T4).
This can be associated with reproductive problems as well as metabolic abnormalities.
Patients with subclinical hypothyroidism are at an increased risk of developing overt hypothyroidism and some believe that these patients should be treated the same as patients with hypothyroidism.
Common symptoms of hyperthyroidism include nervousness, heat intolerance, weight loss, sweating, palpitations, warm-moist skin and goiter (enlargement of thyroid gland).
Subclinical hyperthyroidism is defined as normal thyroid hormone levels and a low TSH level. This condition can be associated with bone loss and atrial fibrillation and therefore needs treatment to prevent cardiac complications and fractures. Progression to overt hyperthyroidism is uncommon, unlike subclinical hypothyroidism.
Whether thyroid disease is overt or subclinical, low or high, it can have a significant impact on reproduction and pregnancy outcome.
It is recommended that thyroid disease screening be done in patients at high risk of having the disease, who are symptomatic, have a significant medical history of autoimmune diseases, history of recurrent pregnancy loss, have ovulation problems or with the presence of thyroid gland enlargement on examination.
In men, hyperthyroidism can cause a marked reduction in sperm count, resulting in infertility. The sperm count usually returns to normal once the thyroid condition has been treated.
Treatment of Thyroid disease
We screen patients for thyroid disease and recommend treatment based on the type of the disorder.
Treatment should be started before pregnancy to improve outcomes and minimize obstetrical complications.

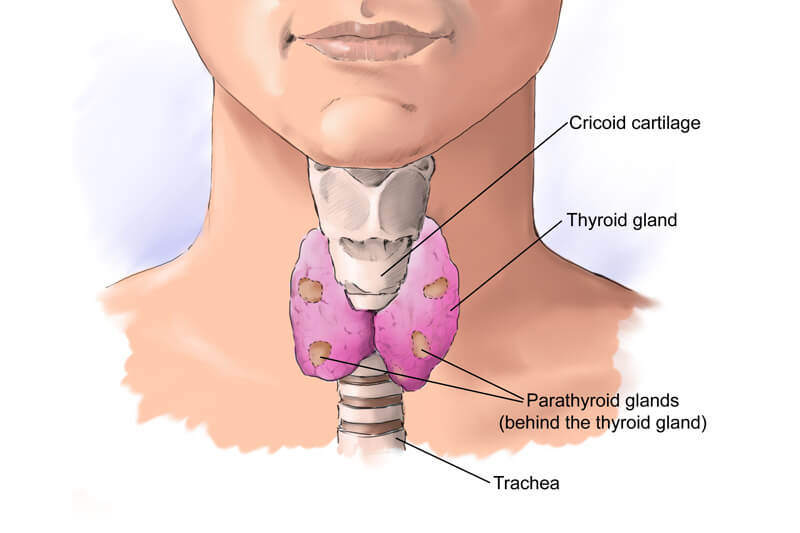
Elevated Prolactin Levels
Earth.com. Image source: What is Pineal Gland? Accessed via https://www.earth.com/earthpedia-articles/pineal-gland/
Hyperprolactinemia is a condition in which a person has higher-than-normal levels of the hormone prolactin in the blood.
The main function of prolactin is to stimulate breast milk production after childbirth, so high prolactin levels are normal in pregnancy.
Prolactin also affects the levels of sex hormones (estrogen and testosterone) in both women and men resulting in irregular menstrual periods and erectile dysfunction, among other things.
Prolactin is made by the pituitary gland, a pea-sized organ found at the base of the brain. At Footsteps To Fertility Centre in Nairobi, Kenya you can expect peace of mind that you are getting assistance from doctors who are experts in the field and have achieved the highest level of fertility training.
Hypothyroidism is commonly treated with levothyroxine (Synthroid, Lovolet, Levoxyl, L-Thyroxine) and hyperthyroidism with propylthiouracil (PTU) or methimazole (Tapazole).
TSH and thyroid hormone levels are checked at regular intervals to sustain normal thyroid function.
Thyroid hormone requirement increases in pregnancy and the dose of supplemental thyroid hormone needs to be increased in patients with hypothyroidism.
Close follow-up and adequate treatment will optimize the outcome.
Once thyroid disease is under good control, patients can attempt to conceive spontaneously or by using assisted reproductive technologies.
Causes of Hyperprolactinemia
One common cause of hyperprolactinemia is a growth or tumor on the pituitary gland called prolactinoma. The tumor produces high levels of prolactin. These tumors can be large or small and are usually benign, meaning they are not cancerous.
Large tumors can also cause headaches, vision problems, or both. Prolactinomas are more common in women than in men and rarely occur in children. Other causes are:
- Hypothyroidism or underactive thyroid—meaning the thyroid gland does not produce enough thyroid hormone
- Chest-wall injuries or other conditions that affect the chest wall, such as shingles
- Other tumors and diseases affecting the pituitary gland, or radiation treatment for tumors on or near the pituitary
- Chronic liver and kidney diseases
Certain prescriptions can also increase prolactin levels. These include medicines for:
- High blood pressure (such as calcium-channel blockers and methyldopa)
- Depression (tricyclic and SSRI antidepressants)
- Heartburn and gastroesophageal reflux disease
- Nausea and vomiting
- Pain (opiates—drugs derived from opium)
- Serious mental health disorders (antipsychotics such as risperdal and haloperidol)
- Menopausal symptoms (estrogen)
Symptoms of Hyperprolactinemia
Both men and women may have infertility, decreased sex drive, and bone loss.
Women may also have:
- Vaginal dryness, leading to pain during intercourse
- Problems with menstruation—having no periods or irregular periods
- Production of breast milk when not pregnant or nursing
Men may also have:
- Erectile dysfunction—trouble getting or keeping an erection
- Breast enlargement called gynecomastia
- Decreased muscle mass and body hair
Diagnosis of Hyperprolactinemia
The diagnosis of hyperprolactinemia involves a routine blood test to check prolactin levels.
If the blood levels are elevated, the doctor may want to repeat the test, this time after fasting for at least eight hours. Normal prolactin levels are less than 500 mIU/L for women and less than 450 mIU/L for men
A magnetic resonance imaging (MRI) scan may be ordered to look for evidence of pituitary growth or for damage to surrounding tissues.
Blood tests to evaluate other hormone levels may be useful in ruling out any other possible causes of the symptoms.
Treatment For Hyperprolactinemia
Treatment is based on the cause. Some people with high prolactin levels, but few or no signs and symptoms, do not need any treatment.
Options for treating tumors include:
- Prescription medicines. Bromocriptine and cabergoline decrease prolactin production. Medicines work well for most people with prolactinomas.
- Surgery to remove a tumor. Surgery may be used if medicines have not been effective. Surgery is sometimes needed if the tumor is affecting vision.
- Radiation. Rarely, if medicines and surgery have not been effective, radiation is used to shrink the tumor.
- Hypothyroidism can be treated with synthetic thyroid hormone, which should bring prolactin levels down.
- If high prolactin levels are caused by prescription drugs, substitute medications may be prescribed.
Excessive Hair Growth (Hirsutism)

Hirsutism is defined as excessive hair growth in various body areas commonly known as “androgen-dependent” sites.
Androgens are a group of hormones present in both males and females, but the levels are much higher in males (ie. testosterone).
Androgen-dependent body sites refer to body areas where males have more hair, including the upper and lower back, lower abdomen, thighs and legs, between breasts, chin and the face.
Excessive hair can be observed in healthy women on the chin, sideburns and above the upper lip.
A severe form of hirsutism is called virilization which presents with the deepening of the voice, male type balding, changes in body habitus and enlargement of the clitoris.
Virilization is due to an excessive amount of androgen production and is generally related to tumors releasing androgenic hormones (adrenal hyperplasia, androgen producing tumors of the ovary and the adrenal gland).
At Footsteps To Fertility Centre in Nairobi Kenya, your health is our priority and we ensure you get all the treatment that you will require towards recovery from Hirsutism.
Women naturally produce male hormones (androgens). Elevated levels of androgens can cause fine, “villous” hair follicles to produce larger, darker “terminal” hair, which leads to hirsutism.
When a woman has more male hormones than normal, it is most often due to a disorder called polycystic ovary syndrome (PCOS).
Hirsutism may be caused by other disorders of male hormone overproduction, but these are not common. Medications such as anabolic steroids that contain male hormones can cause hirsutism.
When a woman has hirsutism but does not have high levels of androgens, this is called “idiopathic hirsutism” because the specific cause of the excessive hair growth cannot be identified.
Another rare disease called Cushing’s syndrome can also result in hirsutism, although other signs and symptoms are common and include high blood pressure, diabetes, muscle weakness, fatigue, red stretch marks and obesity.
Diagnosis Of Hirsutism
It is important to exclude all causes of androgen access especially if there is virilization because the cause may be due to a tumor.
In almost all cases of excessive androgen production related to tumor growth, clinical signs require advanced testing to identify the tumor.
Specific and advanced hormone testing is indicated in such clinical presentations to rule out Cushing syndrome from hirsutism.
Treatment of excessive hair growth
Weight loss is associated with a slight improvement in unwanted hair growth. Women with hirsutism and PCOS should consider making lifestyle changes to improve their overall health.
The choice of treatment depends on the patient’s age, desire for pregnancy or contraception and co-existing metabolic disorders such as insulin resistance.
In most cases, visible effects of hirsutism such as undesired facial and body hair are the most disturbing to the patient.
Most women start with an oral contraceptive (birth control pill) and if they are not pleased with the improvement after six months, a second medication called an antiandrogen can be added. All birth control pills work about the same for hirsutism.
Finasteride is a 5-alpha reductase inhibitor and blocks the production of DHT from testosterone. Testosterone levels are generally not changed and the side effects are rare. Hair growth is less stimulated with finasteride use because the most potent androgen DHT is produced in lower quantities.
Eflornithine (Vaniqa) is an enzyme blocker (ornithine decarboxylase) that has an important role in the development of the hair follicle. Its use has been limited to the face initially, but now it is commonly used in other body areas as well.
The side effects are burning and tingling of the skin, but the drug is generally well tolerated. Once the drug is discontinued beneficial effects are diminished within 8 weeks, which is also the case with other agents.
Mechanical hair removal should be combined with hormonal or non-hormonal treatments and can include shaving, bleaching, using depilatory agents, electrolysis and laser hair removal.
Laser hair removal has been one of the most popular methods recently with high success rates.

Irregular Periods / Menses

Every woman is different, and so are our menstrual cycles. Some of us get them like clockwork, while others are a little less predictable. It can be disconcerting to experience an irregular period.
A typical menstrual cycle tends to vary from 23 to 35 days. Menstrual bleeding is considered irregular if it occurs more frequently than every 21 days or lasts longer than 8 days.
Irregular menstrual bleeding could indicate a health issue, so it’s important to reach out to a doctor if you notice any inconsistencies. Whether you’re concerned about the length, heaviness, or regularity of your period, at Footsteps To Fertility Centre, we specialize in the treatment of irregular menstruation and other hormonal disorders that affect the reproductive system of adolescents and women.
What are considered as irregular periods?
Most women have between 11 and 13 menstrual periods each year. Bleeding usually lasts around 5 days, but this too can vary, from 2 to 7 days.
When menstruation first starts, it can take up to 2 years to establish a regular cycle. After puberty, most women’s menstruation is regular. The length of time between each period is similar.
However, for some women, the time between periods and the amount of blood shed vary considerably. This is known as irregular menstruation.
The main symptom of irregular menstruation is when the cycle is longer than 35 days, or if it comes more frequently than 21 days.
If there are changes in blood flow, or if clots appear that are more than 2.5 centimeters in diameter, this is also considered irregular.
What can cause an irregular period?
Several common factors can affect the rhythm of your cycles. Here are some possible causes of irregular cycles that are also infertility risk factors:
- Polycystic ovarian syndrome (PCOS): Irregular periods may be a sign of polycystic ovarian syndrome (PCOS).
Other illnesses: Thyroid disorders can cause irregular periods if blood levels of the thyroid hormone go too low or too high. Other health conditions that may cause an irregular cycle include sexually transmitted diseases, diabetes, fibroids, and endometriosis. - Birth control: Any changes to your birth control can disrupt your cycles for a few months.
Age. When teens first start having periods, their menstrual cycles may not always be on the same schedule every month. It may take several years to settle into a pattern. In addition, missed periods and lighter or heavier periods are common in women near menopause. - Exercise, dieting & weight fluctuations: Extreme exercise, diet or body weight can contribute to irregular periods. Female athletes are more likely to experience infertility for this reason.
- Stress. Chronic stress or even short-term anxiety about a specific problem can wreak havoc with your hormone balance, causing a missed period and irregular cycle.
When should you be concerned about an irregular period?
A missed or irregular period may be the first clue that you have a condition that needs medical attention. If you have consistently irregular periods, you should be evaluated for PCOS.
You should also be screened for thyroid disorders and other diseases that may be linked to irregular periods.
If you’re concerned about the regularity of your menstrual cycle, an easy first step is to keep a written record of your period.
This record can help set your mind at ease if it turns out that you’re more regular than you realized.
You will also be able to recognize when to take proactive measures. Schedule an appointment with your gynecologist if you experience irregularity over multiple cycles.
During your appointment, the OB-GYN will typically review your medical history with you and might also perform tests such as pelvic exams, Pap tests, MRI or CT scans and minimally invasive hysteroscopy.
An irregular cycle can make it more difficult to get pregnant, especially if you’re not ovulating every month. Your doctor can run tests to see if you’re ovulating. Women with irregular periods who are trying to have a baby are sometimes prescribed fertility drugs to increase ovulation.
Irregular or abnormal ovulation accounts for 30% to 40% of all cases of infertility. Having irregular periods, no periods, or abnormal bleeding often indicates that you aren’t ovulating, a condition known clinically as anovulation. If you’re not ovulating, you can’t get pregnant without the help of fertility treatments.
It is therefore a good idea to be checked out by a doctor just to make sure that nothing serious is going on.
Irregular Periods Treatment
Irregular periods are common but you shouldn’t accept them as normal. At Footsteps To Fertility Centre, our trusted fertility specialist advises that we should pay more attention to our lifestyle. The amount of sleep you get, eating habits and stress level all play an important role in your attempt to get pregnant. Another important thing you can do is to take good care of your health and emotional well-being.
Irregular periods are often a highly treatable condition. Understanding the causes of irregular periods and how you can help to restore cycle regularity can help as you embark on your trying to conceive adventure.
To increase the number of your ovulation period, doctors often prescribe medication and fertility drugs. These drugs induce ovulation that can result in multiple gestations in some women.
Timing intercourse around ovulation can increase your chances for pregnancy since you’ll need to have sex during your fertile window to conceive.
Treatments for patients with irregular cycles
Treatments for menstrual irregularities often vary based on the type of irregularity and certain lifestyle factors, such as whether a woman is planning to get pregnant.
Treatment for menstrual irregularities include:
- Treatments for an underlying disorder that is causing the menstrual problem, such as counseling and nutritional therapy for an eating disorder.
- Oral contraceptives
- Use of various nonsteroidal anti-inflammatory medications
- If the cause is structural or if medical management is ineffective, then gynecologic surgery is recommended. It involves minimally invasive surgical techniques such as surgical removal of polyps or uterine fibroids, uterine artery embolization, endometrial ablation and hysterectomy. They provide a faster recovery and fewer complications than traditional open surgery. These approaches also preserve fertility.
You can count on the extensive experience of the team at Footsteps To Fertility Centre to identify the cause and effectively treat irregular periods.
If you have any questions about your menstrual periods, feel free to contact us or schedule an appointment online.
Book Your
Appointment today!
Make an Appointment